Vitamin D Supplement Sleep
Don't miss out on the latest nutrition and supplement research
Enter your email and we'll keep you on top of the latest nutrition research, supplement myths, and more.
Study under review: The effect of vitamin D supplement on the score and quality of sleep in 20-50 yearold people with sleep disorders compared with control group
You are reading a free Examine article. Become a Member to get full access to all our articles and stay on top of the latest research.
Introduction
The optimal amount of sleep varies from person to person. Most adults require [1] at least seven hours per night on a regular basis. Sleeping less than this is associated with numerous adverse health outcomes, including cardiometabolic diseases, impaired immune function, impaired cognitive performance, and even death. Most people suffering from a lack of sleep tend to also [2] have a lower satisfaction with their economic, social, and family situations, but certain disease states play a role as well. Insomnia is the most common [3] specific sleep disorder, with approximately 30% of adults reporting problems with insomnia and approximately 10% suffering from chronic insomnia.
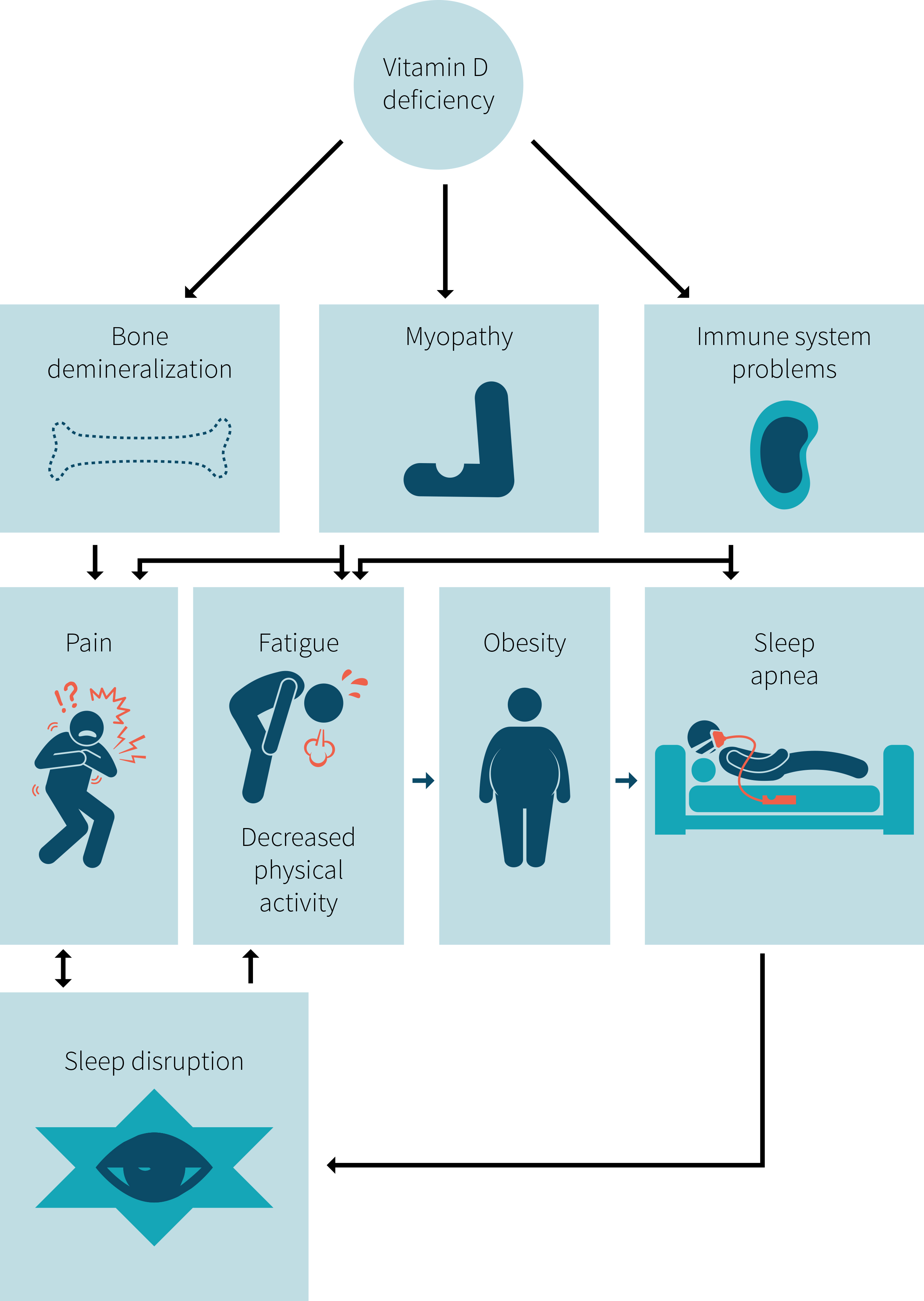
It has recently been hypothesised that vitamin D may play a role [4] in maintaining good sleep and that chronically low levels of vitamin D could result in impaired sleep. Vitamin D's theoretical interactions with sleep are summarized in Figure 1. However, direct investigations of the role of vitamin D supplementation in sleep disorders is lacking. Some studies [5] have shown associations between low vitamin D levels in the blood and sleep quality. Other sleep disorders, such as obstructive sleep apnea [6], have also been associated with lower vitamin D levels. While this limited evidence is primarily observational, meaning we can't be sure about cause and effect, it was enough to inspire the study authors to investigate the potential effect of vitamin D supplementation on sleep quality in a randomised controlled trial.
Poor sleep is a common health concern that can affect quality of life and potentially have negative consequences for an individual's health. Observational evidence has suggested a correlation between sleep quality and vitamin D levels, but the evidence is sparse and interventional evidence is lacking. This study is the first randomised control trial designed to investigate whether vitamin D supplementation improved sleep quality.
Figure 1: How vitamin D deficiency may interact with sleep
Who and what was studied?
This study was a double-blind, randomized controlled trial on 93 people ages 20 to 50 years in a single hospital in Iran. Participants were included if they suffered from poor sleep, as assessed by the Pittsburg Sleep Quality Index (PSQI) [7], a questionnaire that measures sleep quality and disturbances over the previous month. The aspects of sleep the questionnaire assesses are summarized in Figure 2. Poor sleep was defined as a total score of five or more, out of 21, on the PSQI questionnaire, with subsequent confirmation by a doctor that the candidate did not suffer from a specific sleep disorder. A score of five on the PSQI is the cutoff for what is considered poor sleep quality using this metric. Thus, the people enrolled in this trial had poor sleep quality overall, but no identifiable sleep disorder causing it.
Figure 2: Seven components that go into the PSQI score

Participants were excluded if they were smokers, were taking sleep medications, or had taken any high-dose vitamin D supplement in the previous three months. Anyone with health conditions that may cause sleep problems were also excluded. Personal details of the participants were gathered through personal interviews. Sun exposure was estimated at the beginning and end of the study by asking the participants about the duration and parts of the body exposed to the sun and their use of sunscreen.
Participants in the vitamin D group received four doses of 50,000 IU vitamin D3, with one dose every two weeks. This resulted in an average dosage of 3,571 IU of vitamin D3 per day during the study. The placebo group was given a capsule containing edible paraffin oil on the same schedule. Blood samples were taken, and levels of vitamin D in the blood were measured, at the beginning of the study and at the end, after eight weeks of supplementation with vitamin D or placebo. No primary outcomes were specified.
This double-blind, placebo-controlled, randomised controlled trial tested the effect of supplemental vitamin D on sleep quality in Iranian adults with poor sleep. The trial lasted eight weeks. Participants were given a high dose of 50,000 IU vitamin D3, once every two weeks.
What were the findings?
Baseline vitamin D levels were 25 ng/mL (62.5 nmol/L) for the vitamin D group and 27.6 ng/mL (69 nmol/L) for the placebo group. After the eight-week study, levels had significantly increased to 37.7 ng/ml (94 nmol/L) in participants taking the vitamin D and remained unchanged in the placebo group. The between-group difference was significant.
Some of the main findings from the study are shown in Figure 3. The total sleep score at the end of the study was significantly improved in the vitamin D group compared to the placebo group. The score was reduced by 2.7 points in the vitamin D group, falling from 9.45 at baseline to 6.75 by the end of the study, while the total PSQI score did not change significantly in the placebo group from an initial score of 10.51 and final score of 9.7. In this case, a lower score indicates improved sleep quality.
Figure 3: Some results from the study
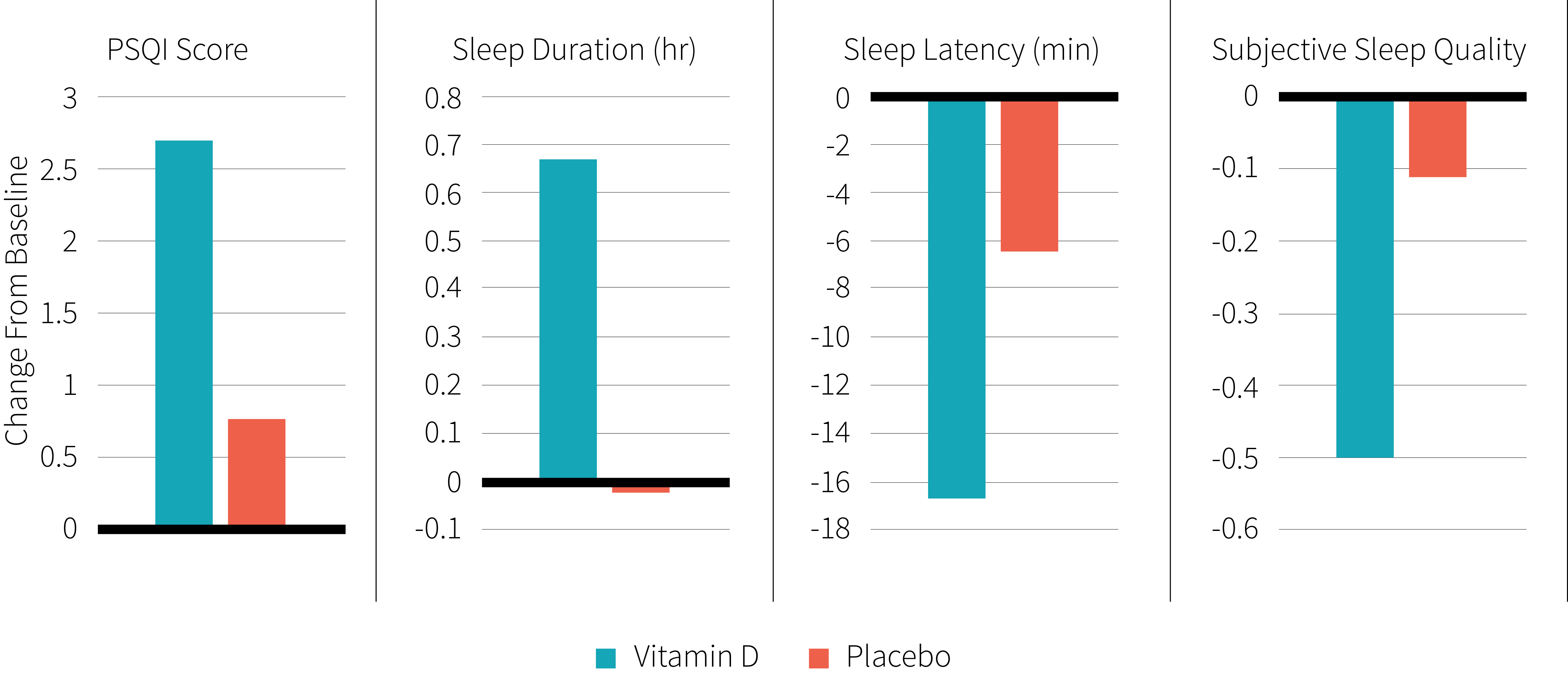
Scores for several aspects of sleep quality measured by the PSQI were improved at the end of the study in the vitamin D group compared to the placebo group, with there being little difference between them at the start. The vitamin D group had a longer sleep duration at the end of the study: 6.5 hours compared to 5.2 hours for placebo. The time it took to fall asleep was 33 minutes for the vitamin D group at the end of the study, compared to 59 minutes in the placebo group. The percentage of time in bed spent asleep was 87% in people treated with vitamin D, compared to 81% for people treated with placebo. Finally, subjective sleep quality scores were 1.2 compared to 1.5 at the end of the study for the vitamin D and placebo groups, respectively, with a lower score indicating better quality sleep. Use of sleep medication and daytime dysfunction scores were not different between the two groups.
The reported minutes of sun exposure each day was the same in both groups at the start of the study and slightly but significantly reduced in the group taking vitamin D (from 21 to 17 minutes), while remaining unchanged in the placebo group. The number of minutes that participants spent napping each day and levels of physical activity were similar between both groups and was not altered by either intervention.
There were no significant differences in measurements such as bodyweight, body mass index, waist circumference, hip circumference, and waist-to-hip ratio between the vitamin D and placebo groups at the beginning or end of the study. Age, sex, education, and marital status were similar between the two groups.
The sleep quality scores improved in participants taking the vitamin D supplement while remaining unchanged in placebo group. Blood levels of vitamin D increased in those taking the supplements, but not in the placebo group. The vitamin D group had a significantly greater improvement in sleep quality than the placebo group
What does the study really tell us?
This is the first trial to investigate the effects of vitamin D supplementation on sleep quality in individuals without other specific medical conditions. The increase in vitamin D levels in the blood of participants in the vitamin D group confirmed that the participants actually took the pills and that they were effectively absorbed. This is a promising exploratory trial that provides suggestive evidence that supplemental vitamin D may help improve sleep in younger people who are vitamin D insufficient without other identifiable sleep problems. Although the study has limitations, it may be enough to warrant future, larger, more carefully focused investigations.
One such limitation is the clinical relevance of its findings, since it is difficult to determine what the decrease of 2.7 in total sleep quality score found in this study would mean at the practical level. The PSQI questionnaire [7] uses a cut-off of five or more to define poor sleep and, by this measure, the average post-intervention score of 6.75 would mean those in the vitamin D group would still be considered to have poor sleep at the end of the study, on average. However, an improvement of 2.7 in the total sleep quality score is more than half the score needed to be classified as a poor sleeper, so it's quite possible that this could make a practical impact on sleep quality for some people. However, the results presented in the study under review make this hard to know for certain.
The use of the PSQI as the main metric in this study leads to some other issues concerning study interpretation. Participation was based on an overall PSQI sleep score of five or above. While this is a reliable method of classifying people as poor sleepers, the information it yields is not very detailed. This means that it's difficult to determine why they were sleeping poorly to begin with, or even whether the types of sleep problem differed between the vitamin D and placebo groups. This means that we cannot say from this study whether the potential benefits of vitamin D to sleep apply to any specific sleep problem, such as restless leg syndrome, or sleep apnea.
A limitation of using the PSQI is that it relies solely on self-reported data to evaluate the participants' sleep quality. However, a recent meta-analysis [8] concluded that the PSQI questionnaire is the most commonly used generic sleep measure in clinical and research settings and its results correlate well with other measures of sleep quality, such as a clinical diagnosis of insomnia. While the study sufferers from problems common to self-reported data, it appears to be somewhat reliable. More objective evidence could be obtained in the future by recording participant sleep in a sleep lab.
There's also a question about the generalizability of this study's results. A vitamin D blood level of between 20-29 ng/ml can be considered as insufficient [9], and levels less than 20 ng/ml as deficient, although there is not universal agreement on normal vitamin D levels. Participants had vitamin D levels below 30 ng/ml at the start of the study, suggesting that their vitamin D levels were low, but that they were not deficient. This means any benefits of supplemental vitamin D on sleep may not occur in people with already high levels and raises the possibility that the effects may have been larger in people with lower vitamin D status, although this remains speculative.
High dose vitamin D supplements were used in this study, containing 50,000 units of vitamin D taken once every two weeks. While this is beneficial in helping participants maintain compliance with the study, as they don't have to remember to take a supplement everyday, it may not be as effective as daily supplements. One study reported that a daily dose of vitamin D [10] was more effective than weekly or monthly doses at correcting vitamin D deficiency. Thus, it's possible that daily supplementation may more effectively increase vitamin D levels compared to less frequent dosing. This, in turn, may also lead to different effects on sleep quality, and would also more closely mimic how a lot of people actually take vitamin D. Future studies using daily dosing are warranted.
This study was relatively short for studies involving vitamin D supplementation, as the level of this vitamin accumulates gradually in the body. Previous studies have found [11] that vitamin D levels in the blood increase and then plateau after supplementation in people deficient in vitamin D. This would indicate that the participants were only just reaching their new higher level of vitamin D by the final week of the study, potentially limiting any beneficial effects. A longer study with more participants would be useful in addressing this.
This study tells us that the vitamin D supplementation may improve sleep quality in people who have moderately low levels to begin with. However, this study cannot say how vitamin D might benefit sleep or whether these benefits may extend to people with specific sleep problems. While these benefits for sleep quality were statistically significant and suggest a meaningful benefit, determining the real world relevance of these improvements will require more research.
The big picture
Vitamin D has recently been hypothesised to have a role in sleep regulation [4], with vitamin D potentially reducing inflammatory cytokines that can interfere with sleep, reducing the risk of other medical conditions that interfere with sleep, or acting directly on parts of the brain involved in regulating sleep. The results of this study suggest that this hypothesis may have some clinical merit. Increasing evidence suggests that vitamin D is involved in brain function [12] and vitamin D receptors are found in several regions of the brain [13] involved in sleep such as the preoptic area of the hypothalamus [14]. This hints that vitamin D could potentially influence the function of areas of the brain controlling sleep. Another potential mechanism is the ability of vitamin D to influence the immune system. Vitamin D can reduce inflammation [15] which reduces the production of prostaglandin D2, an inflammatory signalling molecule that has a role in sleep regulation [16].
Low levels of vitamin D may disrupt sleep indirectly by increasing the risk of other medical problems that disrupt sleep. Vitamin D deficiency has been reported in sleep apnea [17] and vitamin D levels are inversely related to its severity [6]. However, a recent study found [18] that treating sleep apnea increased vitamin D levels in the blood, suggesting that the interactions between sleep apnea and vitamin D may be complex.
Severe vitamin D deficiency has also been reported in people with persistent, nonspecific musculoskeletal pain [19], which can negatively affect sleep. Vitamin D supplementation has been shown to improve chronic pain and sleep quality [20] in a small uncontrolled trial of U.S. veterans with low vitamin D levels who were suffering from chronic pain. These veterans also experienced reductions in pain, the amount of time it took to fall asleep, and increased sleep duration. However, sleep apnea or chronic pain is unlikely to have played a role in the present study as participants suffering from specific medical problems were not included.
Correlations between vitamin D status and sleep have also been reported in several populations. Shorter length of sleep [21] is associated with lower vitamin D levels in the blood and low blood levels of vitamin D have been independently associated [5] with sleep disturbance in hemodialysis patients. In elderly Koreans, higher blood vitamin D levels were positively associated with longer sleep duration [22]. Among older men, low levels of blood vitamin D were associated with poorer sleep [23], including short sleep duration and a smaller percentage of time in bed spent asleep. As these were just associations, it is impossible to conclude whether low vitamin D was involved causally, or merely correlated with poor sleep. One possible confounder is that people who are healthier could get outside more and get more exercise, possibly resulting in better overall health, including better sleep and higher vitamin D levels. These studies were also done in fairly narrow populations. More research is needed to see if these associations hold up in the general population.
There are correlations between low blood vitamin D and poor sleep. There are also potential mechanisms through which vitamin D could influence sleep, either directly acting on the brain or immune system, or indirectly reducing sleep-disrupting health problems, although individuals with these health problems were not included in the study under review.
Frequently asked questions
Q. How does sun exposure influence sleep?
Sunlight exposure does not just result in vitamin D production in our skin. It can also directly influence sleep quality through its effects on our circadian rhythms [24]. Increased exposure to sunlight in elderly nursing home residents [25] can improve sleep quality scores. Similarly, workers in windowless offices [26] suffered from poorer sleep quality than those working by windows. For workers in Antarctica in the winter [27], the benefits of light can be produced using bright sun lamps, which make up for the negative effects of under-exposure of sunlight [28] on sleep. So, it seems that increased sun exposure could benefit sleep quality both through improved circadian rhythms and also increased vitamin D levels. Therefore, sun exposure is a confounding factor when studying the relationship between vitamin D levels and sleep.
What should I know?
Poor quality sleep is a common problem that can affect health and quality of life. This clinical trial suggests that, compared to placebo, a high fortnightly dose of supplemental vitamin D can improve the sleep quality of individuals with poor sleep quality and moderately low, but not deficient, vitamin D levels. However, the improvements were modest and did not completely resolve the participants' poor sleep quality. Larger trials with a longer duration and direct measurements of sleep quality are required to confirm these benefits. Trials examining daily dosing of vitamin D may also be useful.
You are reading a free Examine article. Become a Member to get full access to all our articles and stay on top of the latest research.
See other articles with similar topics: Vitamin D, Sleep.
See other articles in Issue #34 (August 2017) of Study Deep Dives.
Other Articles in Issue #34 (August 2017)
- Interview: Brandon Roberts, PhD
In this volume, exercise scientist, coach, and research consultant Brandon Roberts talks with us about common mistakes he sees in strength training, the state of exercise science, and more.
- Interview: Phil Graham, BSc, PGDip, CISSN, MSc(c)
Phil Graham lives and thrives with type 1 diabetes. In this interview, we pick his brain about his body building experience, tips for professionals working with athletes with type 1 diabetes, and the interactions between insulin, dietary protein, and muscle protein synthesis.
- Beef protein: anabolic underdog?
Whey protein supplementation is considered a top contender when in comes to improving resistance training outcomes. Can a protein supplement derived from beef compete?
- Lean beef: take it or leave it for weight loss
High-protein diets are one way to shed some pounds. Is red meat any better or worse of a protein source for those looking to lose weight?
- Is there really no benefit from protein supplementation on weight loss maintenance?
There's reason to think that protein supplementation can be helpful for weight loss. The question of whether it's useful in weight maintenance is another matter
- The effect of protein supplementation on muscle mass and strength
A recent systematic review has questioned the long-standing belief that protein supplementation can help improve strength training outcomes. This metaanalysis quantitatively examines the latest evidence on the issue
- Ginger, vitamin B6 , or neither for nausea during pregnancy?
Ginger and vitamin B6 are commonly thought to be helpful for nausea and vomiting during pregnancy. Few trials have looked at them head-to-head, though.
References
- ^ Watson NF, et al. Recommended Amount of Sleep for a Healthy Adult: A Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. (2015)
- ^ Rowshan Ravan A, et al. Thirty-six-year secular trends in sleep duration and sleep satisfaction, and associations with mental stress and socioeconomic factors--results of the Population Study of Women in Gothenburg, Sweden. J Sleep Res. (2010)
- ^ Ferrie JE, et al. Sleep epidemiology--a rapidly growing field. Int J Epidemiol. (2011)
- ^ a b McCarty DE, et al. The link between vitamin D metabolism and sleep medicine. Sleep Med Rev. (2014)
- ^ a b Han B, et al. Association between Serum Vitamin D Levels and Sleep Disturbance in Hemodialysis Patients. Nutrients. (2017)
- ^ a b Bozkurt NC, et al. The relation of serum 25-hydroxyvitamin-D levels with severity of obstructive sleep apnea and glucose metabolism abnormalities. Endocrine. (2012)
- ^ a b Buysse DJ, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989)
- ^ Mollayeva T, et al. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: A systematic review and meta-analysis. Sleep Med Rev. (2016)
- ^ Holick MF. Vitamin D deficiency. N Engl J Med. (2007)
- ^ Chel V, et al. Efficacy of different doses and time intervals of oral vitamin D supplementation with or without calcium in elderly nursing home residents. Osteoporos Int. (2008)
- ^ Schleck ML, et al. A Randomized, Double-Blind, Parallel Study to Evaluate the Dose-Response of Three Different Vitamin D Treatment Schemes on the 25-Hydroxyvitamin D Serum Concentration in Patients with Vitamin D Deficiency. Nutrients. (2015)
- ^ Groves NJ, McGrath JJ, Burne TH. Vitamin D as a neurosteroid affecting the developing and adult brain. Annu Rev Nutr. (2014)
- ^ Eyles DW, et al. Distribution of the vitamin D receptor and 1 alpha-hydroxylase in human brain. J Chem Neuroanat. (2005)
- ^ Szymusiak R, et al. Preoptic area sleep-regulating mechanisms. Arch Ital Biol. (2001)
- ^ Wang Q, et al. Vitamin D inhibits COX-2 expression and inflammatory response by targeting thioesterase superfamily member 4. J Biol Chem. (2014)
- ^ Urade Y, Hayaishi O. Prostaglandin D2 and sleep/wake regulation. Sleep Med Rev. (2011)
- ^ Kerley CP, et al. Serum Vitamin D Is Significantly Inversely Associated with Disease Severity in Caucasian Adults with Obstructive Sleep Apnea Syndrome. Sleep. (2016)
- ^ Liguori C, et al. Continuous Positive Airway Pressure Treatment Increases Serum Vitamin D Levels in Male Patients with Obstructive Sleep Apnea. J Clin Sleep Med. (2015)
- ^ Plotnikoff GA, Quigley JM. Prevalence of severe hypovitaminosis D in patients with persistent, nonspecific musculoskeletal pain. Mayo Clin Proc. (2003)
- ^ Huang W, et al. Improvement of pain, sleep, and quality of life in chronic pain patients with vitamin D supplementation. Clin J Pain. (2013)
- ^ Darling AL, Skene DJ, Lanham-New SA. Preliminary evidence of an association between vitamin D status and self-assessed sleep duration but not overall sleep quality: results from the D-FINES study of South Asian and Caucasian pre- and post-menopausal women living in Southern England. Proceedings of the Nutrition Society. (2011)
- ^ Kim JH, et al. Association between self-reported sleep duration and serum vitamin D level in elderly Korean adults. J Am Geriatr Soc. (2014)
- ^ Massa J, et al. Vitamin D and actigraphic sleep outcomes in older community-dwelling men: the MrOS sleep study. Sleep. (2015)
- ^ Wright KP Jr, et al. Entrainment of the human circadian clock to the natural light-dark cycle. Curr Biol. (2013)
- ^ Düzgün G, Durmaz Akyol A. Effect of Natural Sunlight on Sleep Problems and Sleep Quality of the Elderly Staying in the Nursing Home. Holist Nurs Pract. (2017)
- ^ Boubekri M, et al. Impact of windows and daylight exposure on overall health and sleep quality of office workers: a case-control pilot study. J Clin Sleep Med. (2014)
- ^ Mottram V, et al. The impact of bright artificial white and 'blue-enriched' light on sleep and circadian phase during the polar winter. J Sleep Res. (2011)
- ^ Smolensky MH, Sackett-Lundeen LL, Portaluppi F. Nocturnal light pollution and underexposure to daytime sunlight: Complementary mechanisms of circadian disruption and related diseases. Chronobiol Int. (2015)
Source: https://examine.com/members/deep-dives/article/can-supplemental-vitamin-d-improve-sleep/

Tidak ada komentar: